A novel type of hospital is being introduced to rural areas of America, lacking the provision of inpatient beds.
In the United States, rural hospitals are facing financial challenges and a newer type of hospital is emerging, particularly in the Southeast region.
Rural emergency hospitals receive more than $3 million in federal funding a year and higher Medicare reimbursements in exchange for closing all inpatient beds and providing 24/7 emergency care. While that makes it easier for a hospital to keep its doors open, experts say it doesn’t solve all of the challenges facing rural health care.
Some individuals may need to journey longer distances in order to receive treatment for certain illnesses that necessitate hospitalization, such as pneumonia or COVID-19. In areas where hospitals have changed to the new status, there is confusion among residents about the level of care available. Additionally, rural hospitals are hesitant to transition due to the lack of room for mistakes.
Carrie Cochran-McClain, the chief policy officer at the National Rural Health Association, expressed the irony that the very facilities in need of assistance are unable to afford the risk of seeking it. She cited examples such as having to forego essential services and benefits, such as a federal program for discounted prescription drugs.
In January 2023, the government introduced a new classification system for hospitals, including a rural emergency option. The University of North Carolina’s Sheps Center for Health Services Research reported that nineteen hospitals in the United States were designated as rural emergency hospitals last year.
Most of them are located in the southern region, while a few can be found in the midwestern states.
George Pink, deputy director of the Sheps Center’s Rural Health Research Program, stated that the designation targets a highly specific demographic, namely rural hospitals that are on the verge of shutting down and have minimal numbers of patients receiving inpatient care.
Saving rural care
This applied to the Irwin County Hospital in Ocilla, Georgia, which became the second emergency hospital set up in rural areas across the United States.
Before the conversion, the hospital was given a minimum of $1 million in credit from the county in order to compensate its employees. County board of supervisors’ chairman Scott Carver was unsure if this money would be repaid.
According to the speaker, our county’s budget is $6 million and offering such a large credit line was risky. However, we felt it was necessary to take the chance.
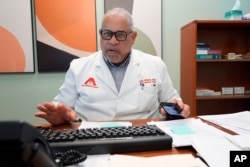
On February 1, 2023, Irwin County Hospital transitioned into a rural emergency hospital. According to CEO Quentin Whitwell, it was the perfect fit for the hospital.
“We are currently investigating the effects of this new concept,” remarked Whitwell, the owner and manager of six hospitals in the Southeast under Progressive Health Systems. Most of these hospitals are either rural emergency hospitals or in the process of applying for that status. “However, this hospital has seen a significant transformation since becoming a rural emergency hospital.”
According to Carver, a combination of state initiatives and tax incentives, as well as a new designation, has resulted in the hospital having $4 million in funds. In his opinion, the effort put into the work was well worth it.
Traci Harper, a resident of Ocilla for many years, is uncertain. Approximately a year ago, she took her son to the hospital for urgent treatment for spinal meningitis.
Due to the new protocol, patients must be transferred to larger hospitals within 24 hours. As a result, Harper’s son was relocated to a different hospital in the same state and ultimately received necessary treatment at a hospital in Jacksonville, Florida three days later.
She said, “It’s a two hour drive. I could have brought him there myself during that time, but no one informed me.”
Barely surviving
In the town of Friend, Nebraska, the first emergency hospital catering to rural areas opened its doors in February.
Warren Memorial Hospital had reached a critical juncture as the funding from federal pandemic relief had been depleted. The city, as the owner of the hospital, had to provide lines of credit in order for employees to receive their salaries. The hospital’s chief financial officer and one of the three co-CEOs, Jared Chaffin, also mentioned that a significant street repair project had to be put on hold due to the financial strain.
During the summer, we were barely managing to stay afloat,” stated Amy Thimm, the hospital’s vice president of clinical services and quality and co-CEO.
Despite the reservations voiced by citizens during the September meeting regarding the potential closure of inpatient services, the significance of having access to emergency care prevailed over any other concerns.
Ron Te Brink, co-CEO and chief information officer, stated that there are farmers, ranchers, and other busy individuals who are unable to travel long distances for medical care. As a result, they often forego seeking treatment altogether. This highlights the significance of rural health care in communities such as ours in Nebraska.
On March 5th, the initial federal payment of approximately $270,000 was received. According to Chaffin, the hospital is projected to generate a revenue of $6 million this year, which is the highest amount in its history.
“The situation is unbelievable, especially for our small hospital,” he remarked. “We still have a long way to go and a lot of work ahead of us. The designation itself is not a solution for the hospital – it’s a vital support.”
Rural troubles
The task of retaining that vital support has been challenging for Alliance Healthcare System, located in Holly Springs, Mississippi. This facility, which is one of Whitwell’s hospitals and the fourth in the nation to transition, has experienced difficulties.
Several months after being granted as a rural emergency hospital in March 2023, the Centers for Medicare and Medicaid Services reversed their decision.
CEO of the hospital, Kenneth Williams, informed the Associated Press that according to the government, the hospital does not qualify as rural as it is within an hour’s distance from Memphis. A spokesperson from CMS stated that the certification of the facility was a mistake.
According to Williams, the hospital must return to full operation by April, but most of the retired residents in the community think the hospital has shut down. Patient numbers are currently at an all-time low. Williams has doubts about the hospital’s future survival if the government payments cease.
“If we hadn’t become a rural emergency hospital, we may have had to close down. Therefore, we had to take action,” he stated. “Do I have any regrets about the challenges that we have faced, while others [hospitals] have not? I am uncertain.”
Although Alliance appears to be one of few facilities that have been negatively affected by converting to a rural emergency hospital, Pink said it’s too soon to know if the federal designation is a success.
He stated that if my intuition is accurate, it may be successful for certain communities but may not be as effective for others.
Source: voanews.com